(revised on 12 may 2013)
Since 2003, the patent product of Sun Yat sen University automatic hemorrhoid ligation device (also known as continuous hemorrhoid ligation device) and its supporting technology RPH have been gradually popularized and applied in the whole country, and are welcomed and praised by clinical experts and doctors all over the country. However, there are some clinical problems in a few areas, especially in the academic issues such as RPH theory and practice. Now the common and common academic questions in different places are extracted and summarized, and the answers are as follows, for reference only.
1. How does hemorrhoids occur“ What kind of structure is anal pad?
There are two theories about the occurrence of hemorrhoids: "varicose vein theory" and "anal pad downward theory". According to the theory of varicose veins, hemorrhoids are protuberant venous masses formed by tortuous and dilated venous plexus at the end of rectum or subcutaneous venous plexus of anal canal. Internal hemorrhoids are caused by varicose veins at the end of rectum; External hemorrhoids are formed by subcutaneous varicose veins of anal canal; Mixed hemorrhoids (internal hemorrhoids develop into mixed hemorrhoids when they reach grade III or IV) are formed by varicose veins and continuous raised venous mass connecting the end of rectum and the subcutaneous layer of anal canal. According to the theory of anal pad downward movement, hemorrhoids are formed when the supporting structure of anal pad relaxes, breaks, becomes hypertrophy, moves downward and prolapses, and the venous plexus is tortuous and dilated at the same time. These two theories complement each other. In April 2000, the group of anorectal surgery, Chinese society of surgery, Chinese Medical Association formally defined hemorrhoids as "local mass formed by pathological hypertrophy and displacement of anal pad and blood stasis of perianal subcutaneous vascular plexus".
Of course, the incidence of hemorrhoids is very complex, far from the above two theories can include, pelvic floor hemodynamic changes, abdominal pressure changes, venous reflux disorders, local infection, inflammation, eating habits, etc., may play a role in the incidence of hemorrhoids.
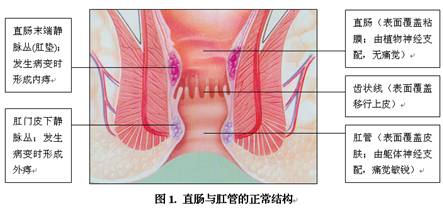
So, what is "anal pad"? In normal people, there is a special tissue structure under the mucous membrane of anal canal and rectum end, which is composed of blood vessels, smooth muscle (Treitz muscle), elastic fiber and connective tissue. It has been formed in the fetus. Its function is to assist the normal closure of anus and play the role of coordinating and controlling defecation (just like the "washer of faucet"), This structure is called "anal pad" in medicine (as shown in Figure 1). Under normal circumstances, the anal pad is loosely attached to the muscle wall of the rectum and anal canal, pushed down by abdominal pressure during defecation, and then retracted back to the anus with its own contraction after defecation. However, when the anal pad is congested, hypertrophic, relaxed and broken, its elastic retraction is weakened, which gradually moves down and prolapses, and leads to blood stasis and varices in the venous plexus, forming hemorrhoids over time.
2. What is the treatment of hemorrhoids? What's the status of apron ligation in the treatment of hemorrhoids?
The incidence rate of hemorrhoids is very high. According to the survey, the incidence rate of hemorrhoids in China's population is as high as 87.5%. Hemorrhoids treatment methods are various, such as drugs, injection, rubber band ligation, freezing, radio frequency, microwave, infrared, surgery and so on, each has its advantages and disadvantages. However, the clinical studies of large number of cases in Europe and the United States show that among many treatments, the effect of rubber band ligation is the best. In the United States, Europe and Japan and other developed countries, apron ligation has been the preferred treatment for hemorrhoids. On the contrary, PPH is rarely used in these countries.
The following are some well-known foreign anorectal experts' evaluation of "rubber band ligation" articles, which are very representative and fully illustrate the important position of "rubber band ligation" in the treatment of hemorrhoids.
l. In 1998, MacRae considered that the rubber band ligation is the most effective non-surgical treatment for hemorrhoids (1).
2. In 1999, Salvati summarized 45000 cases of SNARE ligation. Only one case was infected and cured by antibiotics; Among the 595 patients followed up, the 5-15 year symptom control rate was 80% (2 / 595).
3. In 1999, O'Regan wrote that ligation therapy was called the truly minimally invasive technique for the treatment of hemorrhoids by European and American scholars (3).
4. In 2000 and 2003, Kanellos and Peng respectively wrote that ligation therapy is a safe, effective, cheap and convenient method for the treatment of hemorrhoids (4, 5).
5. In September 2005, golden Berge, Professor of the University of Minnesota and President of anorectal surgery of the United States, came to China to give a lecture. He pointed out that ligation therapy has fewer complications and satisfactory long-term effect in the treatment of "hemorrhoids bleeding / prolapse".
——————————————————
reference:
(1) MacRae HM, McLeod RS. Comparison of hemorrhoidal treatments: a meta-analysis. Can J Surg1997,40:14-17.
(2) Salvati EP. Nonoperative management of hemorrhods: evolution of the office management of hemorrhoids. Dis Colon Rectum,1999 Aug; 42(8):989-993.
(3) O’Regan PJ. Disposable device and a minimally invasive technique for rubber band ligation of hemorrhoids.
Dis Colon Rectum. 1999,42(11): 1509-10.
(4) Peng BC, Jayne DG, Ho YH. Randomized t rial of rubber band ligation vs.stapled hemorrhoidectomy for prolap sed piles.Dis Colon Rectum. 2003,46(3) :29127.
(5) Kanellos I, Goulimaris I, Vakalis I, Long-term results of rubber-band ligation for second-degree hemorrhoids:
a prospective study. Tech Coloprocto, 2000,4:992101.
3. What is RPH? What are the similarities and differences with traditional rubber band ligation? What are the advantages?
The traditional rubber band ligation is to tie the rubber band to the base of internal hemorrhoids with some simple instruments, and use the elastic contraction of the rubber band to block (or partially block) the blood supply of hemorrhoids or reduce the backflow of hemorrhoid veins, so as to reduce the congestion and hypertrophy or blood stasis of hemorrhoids, and make the hemorrhoids atrophy and fall off. However, the instruments used for traditional rubber band ligation are very simple and backward. The rubber band can only be used in a single shot (i.e. the operator has to suspend the operation for each shot of rubber band, take out the anal speculum and ligation device, and install the next shot by the assistant). This operation is not only time-consuming and laborious, but also extremely difficult to expose, and sometimes it needs to be completed under anesthesia, It is easy to cause misoperation and complications.
In view of the shortcomings of traditional ligation, Professor Xu Ruiyun of Sun Yat sen University invented a new instrument for ligation of hemorrhoids - automatic ligation device for hemorrhoids (also known as continuous ligation device for hemorrhoids). Since then, it has been improved for many times, and has won the national patent for many times (patent No.: zl03223818.5; patent No.: zl03223818.5; patent No.: zl03223818.5); ②ZL200520061355.8; ③ZL200820051521.X; ④ZL201020644006.X)。 At the same time, Professor Xu Ruiyun also created the hemorrhoid ligation technology with automatic hemorrhoid ligation device automatic hemorrhoid ligation, namely RPH, which standardizes, improves and perfects the traditional ligation method (see Note 1 for the explanation of RPH).
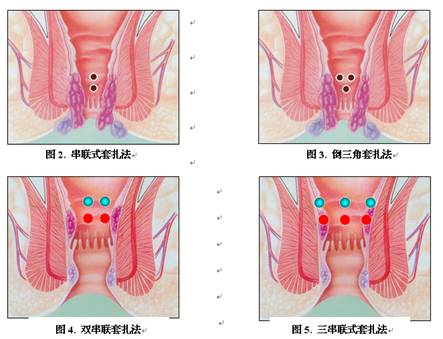
RPH is an innovation of the traditional ligation technology. Compared with the traditional ligation, RPH has many advantages: ① the rubber ring can be used continuously (without repeated installation), the ligation process is fully automated, which is very time-saving, labor-saving and simple. It can be completed by a single person, and takes only 5-10 minutes; Moreover, there is no need for anesthesia and hospitalization, and the price is quite cheap; ② The traditional simple "hemorrhoid block base ligation method" was changed, and "hemorrhoid mucosa ligation method" was created. The hemorrhoid mucosa ligation method was organically combined with hemorrhoid block base ligation method, and "series ligation method", "inverted triangle ligation method", "double series ligation method" and "three series ligation method" were invented (for detailed explanation of ligation method, see below). This new ligation technique takes into account both the "blood stasis" and "anal pad down" two kinds of hemorrhoids pathogenesis, not only the curative effect is greatly improved, but also the pain is very small, and the complications are rare; ③ No scar was left after operation, and the structure and appearance of rectum and anal canal were not damaged, which brought great convenience for follow-up treatment; ④ It can be used repeatedly.
————————————————
Note 1: RPH is the abbreviation of Ruiyun procedure for hydrocarbons, where Ruiyun is the Pinyin name of the inventor Professor Xu Ruiyun.
4. How to operate RPH?
There are two kinds of ligation methods for RPH, namely "hemorrhoid block base ligation" and "hemorrhoid mucosa ligation". The former is the mucosa at the base of the hemorrhoid block (the central point of ligation is about 1.0 cm on the dentate line, which is equivalent to the upper part of the hemorrhoid block); After ligation, the distance between the lower edge of the apron and the dentate line is about 0.5cm; The latter is the rectal mucosa above the ligated hemorrhoids (3-4cm above the dentate line, without ligating the hemorrhoids); After ligation, the lower edge of the apron is about 2.0cm away from the dentate line. For mild and moderate hemorrhoids, hemorrhoids block base ligation method is generally used; For severe hemorrhoids, the combination of hemorrhoid block base ligation and hemorrhoid mucosa ligation has better effect.
There are four combined modes of hemorrhoid block base ligation and hemorrhoid upper mucosa ligation: ① series ligation, that is, ligating a point at the base of hemorrhoid block (1.0cm on the dentate line), ligating another point directly above it (3-4cm on the dentate line) (as shown in Figure 2); ② Inverted triangle ligation method: ligate a point at the base of hemorrhoid mass, form an isosceles triangle above it, and then ligate two points (as shown in Figure 3); ③ Double series ligation method: make two series ligation methods continuously (as shown in Figure 4); ④ Three series ligation method: make three series ligation methods continuously (as shown in Figure 5).
The location of ligation is generally 3, 7-8 and 11-12 points (i.e. 1-2, 5-6 and 9 points) of lithotomy position, which can also be determined according to the specific location of hemorrhoids. A treatment can be ligated 2-3 points (Beginners had better not more than 3 points; However, the skilled person can choose the number of ligation points according to the prolapse of hemorrhoid mass (5-6 points at most). If the hemorrhoid mass retraction is not complete in one treatment, the treatment can be repeated. The interval between two treatments should be more than 4 weeks, until the symptoms improve or disappear. Ligation therapy can also be combined with injection therapy, the specific technical essentials are detailed below.
Different types of hemorrhoids can refer to the following ligation methods:
Choice of ligation method for prolapse degree of hemorrhoids
Single hemorrhoids without or slight prolapse (stage 1-2) single point hemorrhoids block base ligation
The more obvious prolapse (stage 3) was treated with single point tandem ligation
Very serious prolapse (stage 4) or hemorrhoid mass wide single point inverted triangle ligation or double series ligation
Multiple hemorrhoids without or mild prolapse (stage 1-2) three points (maternal hemorrhoids) base ligation
Severe prolapse or annular prolapse (stage 3-4) three-point (maternal hemorrhoid) series ligation
Annular prolapse + Giant external hemorrhoids (stage 4) three point series ligation + external hemorrhoidectomy
5. What are the technical essentials of RPH?
According to the investigation, there is still a certain bleeding rate (0.3% - 2%) after RPH, and it mostly occurs in beginners. In order to reduce the incidence of bleeding complications, we should master the following technical essentials
(1) The ligation point should be 1.0cm on the dentate line. After ligation, the lower edge of the rubber ring should be about 0.5cm away from the dentate line. Do not set too low to avoid ligating the anal column or anal papilla. Otherwise, it is not only prone to postoperative severe distension and urgency, but also the postoperative bleeding rate is relatively high.
(2) Do not use too little tissue. Generally speaking, the ligation tissue should be at least the size of the end of the little finger. If there is too little tissue, the apron will not be firmly tied and easy to slip. The technique of inserting enough tissue is that when the gun barrel is aimed at the target and begins to attract, the gun barrel should be gently pumped back and forth while attracting, so that more and more tissue can be inhaled (pay attention not to suck against the intestinal wall, because less tissue can be inhaled and the rubber ring is easy to slip).
(3) After the apron is fired, when the negative pressure switch is turned on and the ligated tissue is released, the action should be carried out slowly. The gun barrel can be pulled out slowly only when the pointer of the negative pressure gauge is close to zero. Do not act too fast. Otherwise, if the action is rough, the rubber ring may be taken out of the body.
(4) In order to prevent slippage and postoperative bleeding, 1-2ml of "Xiaozhiling injection" or "Xiaozhiling + 2% lidocaine" 1:1 or 2:1 mixture can be injected into the ligated tissue ball after ligating the hemorrhoid tissue with the rubber ring. After injection, the tissue ball was obviously swollen and white, and the rubber ring was tight, which made it difficult to slip. Secondly, Xiaozhiling can promote tissue sclerosis and collapse, accelerate vascular occlusion and organization, and significantly reduce the incidence of postoperative bleeding. In addition, due to the anesthetic effect of lidocaine on peripheral nerves, the feeling of swelling and urgency after ligation will also be significantly reduced.
(5) Be careful not to tie the anal column or anal nipple. Internal hemorrhoids occur in the area of 2cm above the dentate line (i.e. anal pad). If the ligation position is too low, not only the anal pad will be damaged, but also it is too close to the dentate line, so it is easy to insert the anal column or dentate line. The perianal column and dentate line are covered by transitional epithelium (not mucosal epithelium). The healing of transitional epithelium is slow, the incidence of bleeding is high, and the feeling of distention and urgency is also very obvious. If you tie the dentate line or anal skin (showing severe swelling or pain), you should remove the rubber ring as soon as possible to avoid tissue necrosis, delayed healing, infection, massive bleeding and other complications.
(6) Generally, there should be no more than 3 ligation points on the same horizontal plane, otherwise the tension may be too high and the tissue is not easy to be inhaled; Even if the tissue was inhaled at that time, it was easy to cause premature slippage due to excessive tension after operation.
(7) It is better not to do anal endoscopy within three weeks after ligation, because the wound healing is not satisfactory within three weeks, repeated friction may lead to bleeding.
(8) After the initial treatment, the patient should be reexamined one month later. If the hemorrhoid mass does not retract completely or the hematochezia does not stop completely, the second ligation (or the third or more ligation) can be performed; The interval should be more than 4 weeks (one month) until the symptoms improve or disappear.
(9) It is very important to use local medicine after operation. It is suggested to use "Taining suppository (Xi'an Janssen)" or "portley ointment (France)" twice a day for 2-3 weeks, which can greatly reduce the incidence of postoperative bleeding. Attention should be paid to avoid the use of traditional Chinese medicine suppository such as "Ma Yinglong Hemorrhoids Suppository" or "Hua Zhi suppository"; According to the investigation, this kind of suppository not only affects the wound healing, but also may induce bleeding. For example, if the basic hospital does not have "Tinian suppository" or "portley paste", it is also possible to use some cheap traditional ointment such as erythromycin ointment or neomycin ointment, and its anti infection and healing cooperation is more positive.
(10) Patients should be asked to empty the stool before operation or induce the stool with kaiseru (but not enema).
(11) After operation, keep the stool smooth (take soft stool medicine such as Maling soft capsule, etc.) as appropriate, fast food such as spicy, alcoholic and other foods, drink more water, and eat more cellulose high food such as vegetables and fruits; It can be used in combination with sitting bath, external ointment or anal medicine suppository; The antibiotics were taken orally for 3-5 days. A few patients who have a sense of urgency or distension after operation can be treated as appropriate.
(12) If external hemorrhoids were removed at the same time with RPH and a phase suture was made with absorbable line, it is not suitable to sit in bath, otherwise, it is easy to break the suture and make the wound shiver.
(11) If some patients have bleeding after operation, they should be asked to return to the hospital as soon as possible. The general problem of small amount of bleeding is not large (it may be hemorrhoids); If the bleeding amount is large, it is necessary to cut the bleeding immediately under the anal endoscope with absorbable suture as "8" suture for hemostasis. Do not use oil gauze to fill or other conservative measures to avoid delay of the disease.
6. what is the operation of PPH? How to evaluate?
PPH is the abbreviation of procedure for prolapse and hemorroids, in which procedure means "operation and operation"; Prolapse means "sagging and sagging"; And hemorroids is the meaning of hemorrhoids and hemorrhoids. The whole phrase is used for prolapse hemorrhoids. Therefore, PPH has defined its application scope literally, that is, it is limited to the treatment of "prolapse hemorrhoids" (i.e. "severe hemorrhoids"), rather than recommended for light and moderate hemorrhoids.
In China, PPH is usually translated as "stapling procedure for prolapse and hemorrhoids" or "procedure for prolapse and hemorrhoids". A surgery which is only suitable for severe prolapse hemorrhoids is widely used in the treatment of general mild and moderate hemorrhoids in China. There are serious questions about its rationality!
PPH was introduced from Italy to China in 2002. The operation was to cut the lower rectal mucosa off a whole circle by a special cutting stapler. The theoretical basis of PPH is the theory of "anal pad moving down". Because the theory can not explain all the hemorrhoids, it is not perfect; Therefore, PPH design has its own limitations.
There are many "nerve receptors" in the lower rectal and anal areas, which perform their own complex functions (such as "defecation reflex", etc.), once the resection may cause various functional damage, a series of complications may be caused. A large number of investigations and studies at home and abroad show that there are many complications of PPH, such as bleeding (even shock), infection, increased stool times, acute and heavy back, no separation of "Qi feces", dirty dung in underwear, incontinence of stool, anal stenosis, persistent pain around anus, etc. Moreover, titanium nails (most domestic instruments are steel nails) of PPH stapler will be permanently retained in the rectum wall as foreign bodies. Under the long-term action of rectal feces and bacteria, the inflammatory reaction may exist for a long time, and the long-term complications are difficult to predict. The fibrosis and sclerosing of rectal wall after PPH are also very difficult. Once hemorrhoids recur, it will be very difficult to follow up treatment.
In addition, the residual foreign body (titanium nail or steel nail) after PPH operation also easily brings various clinical problems, which has attracted the attention of clinical experts at home and abroad. According to the research, titanium nail (steel nail used by many domestic manufacturers) will not fall off after PPH operation, but will remain in the rectum forever. The foreign body inflammatory reaction may exist for a long time, which is an important reason for postoperative infection, chronic anal pain, irregular stool, sense of emergency stool, scarring or hardening of rectum.
Therefore, PPH has been rarely used in developed countries such as the United States, Europe and Japan since 2004.
In conclusion, PPH and RPH are actually two different therapeutic concepts. As a doctor, no matter what diseases are treated, we should consider carefully whether they conform to the following five basic principles:
1. effectiveness principle: is treatment really effective?
2. simplification principle: is the treatment simple enough (of course, on the basis of not affecting the efficacy)? If there is a simple way to solve problems, we will never use complex methods.
3. low cost principle: is the patient paying enough low cost? Including: tissue damage? Function protection? How many complications? Is it serious? wait.
4. forward looking principle: the effect of treatment on the future? What is the impact on follow-up treatment?
5. economic principle: how about the cost performance? Is the effect proportional to the price?
7. how to understand the "low cost principle"?
Among the five principles, the principle of low cost is the most important principle we can easily ignore. Many people always emphasize how well they use the treatment, but no matter what the harm will be after the operation. In fact, these people often rarely or even have not done any follow-up research and follow-up investigation. PPH, for example, is not used (or rarely) in the United States and Europe, although it is good for severe circular hemorrhoids? Because of its too high cost (too many complications, too serious), it is difficult to accept; The recurrence rate is also high, which is 20% - 30% according to foreign research. What is the situation in our country at present? According to the survey, some municipal hospitals have 1000 PPH consumption in a year, and 200-300 cases are less; But the United States from 2000 to more than 10 years, the national PPH consumption is less than 1000 cases, such a sharp contrast, it is really confusing, more worthy of our vigilance and thinking!
In addition, the traditional "external stripping and internal ligation" must also be mentioned. Some people do too much, too much resection, and bring many irreparable complications. Generally speaking, the removal of three parts must be extremely careful, while some people have to remove 4 or 5 parts. Although hemorrhoids are good, the anus is also damaged almost. What function maintenance is to be discussed? Although the external stripping and internal ligation is classic, it is necessary to grasp correctly, and to protect the skin and tooth line of anal canal. Excessive damage to the area is the important reason for the anal stenosis and defecation abnormality. To remind yourself at all times, although it is important to treat hemorrhoids, it is more important to protect the anus function!
Why was tetracycline eliminated? Can't it cure disease? Isn't it working well? No, it's because it has too many side effects and it's not too bad!
Why are streptomycin and gentamicin less used? Especially in children, they don't use it? It's because it has caused too many family tragedies - permanent deafness, permanent kidney damage
8. Is RPH painful after treatment?
The rectum and anal canal are bounded by dentate line. Above the dentate line is the rectum, which is innervated by autonomic nerve and has no pain sensation; Below the dentate line is the anal canal, which is innervated by the somatic nerve and has a keen sense of pain (as shown in Figure 1). Because the ligation point of RPH is set at 1.0cm of the dentate line, it will not tie the anal column and dentate line, so it generally will not cause pain after operation. Only a few patients have a sense of distension or urgency (the closer to the dentate line, the more obvious). The degree varies from person to person. Most of the symptoms are mild and can gradually disappear after a few hours. However, if "Xiaozhiling + lidocaine mixture" is injected into the ligated tissue ball after RPH (see the injection method later), the feeling of distension or urgency will basically disappear.
But it must be noted that the ligation point must not be too low, such as covering the dentate line or anal skin, which can cause severe pain, even necrosis, infection, bleeding, etc.
9. Can RPH cause bleeding? What are the reasons?
According to the investigation, the incidence of bleeding in the early years of traditional rubber band ligation is relatively high, about 0.8% - 15% (References: 1) Salvati EP. Dis colon rectum, 1999 Aug; 2) the incidence of bleeding in the early years of traditional rubber band ligation is relatively high; 42(8):989-993; ②Armstrong DN. Dis colon Rectum, 2003, 46: 179-185.)。 At present, due to the great improvement of the ligation method and the obvious improvement of the quality of the rubber ring, the incidence of bleeding in RPH is reduced to 0.3% - 2%. If "ligation" and "injection" are combined, the incidence of bleeding can be basically eliminated.
The reason for the low incidence of RPH bleeding is that it places the ligation point at 1.0 cm or higher on the dentate line, where the tissue is covered by the mucosa. As we all know, the growth and healing speed of the mucosa is very fast (according to research, the gastrointestinal mucosa can be completely healed about 48 hours after biopsy injury); At the same time of necrosis and shedding of the top mucosa, the basal mucosa almost healed simultaneously, so there was no bleeding after RPH.
But why do clinicians still often reflect bleeding? This is mainly related to the following factors:
(1) Ligation close to the dentate line: because it is too close to the dentate line, it is easy to cover the anal column and even the dentate line together. What is covered here is not the mucosa, but the transitional epithelium, with slow healing and high infection rate, which is the main cause of postoperative bleeding.
(2) Poor quality of aprons: poor quality of aprons, poor elastic retraction force, loose ligation, large ulcer surface after falling off, incomplete closure and organization of root blood vessels, so it is easy to bleed (whether the root blood vessels of the ligated tissue close and organize quickly mainly depends on the elastic retraction force of aprons). At present, there are a lot of ligators on the market which are manufactured by imitating our products. The rubber ring is provided by small private factories in China. It has poor quality, poor elastic retraction force, easy aging and fracture, and high postoperative bleeding rate.
(3) Improper local anal medication after operation: appropriate local anal medication after operation can prevent infection and promote wound healing. Improper medication can easily lead to postoperative bleeding. The commonly used drugs in anus are Taining suppository (Xi'an Janssen), portley ointment (France), erythromycin ointment, neomycin ointment, etc. it is recommended to use them continuously for at least two weeks; Avoid using traditional Chinese medicine suppository such as "Mayinglong Hemorrhoids Suppository" or "Huazhi suppository".
(4) Patient's own reasons: poor tissue healing ability (diabetes, old and weak), poor coagulation function, constipation, diarrhea, drinking, eating spicy, local infection, etc.
10. How to do the bleeding after RPH?
In case of bleeding after RPH, we should first identify whether it is the continuation of hemorrhoid bleeding or the bleeding caused by rubber ring falling off. The former usually has a small amount of blood loss and usually occurs within 1-3 days after operation; The latter has a large amount of bleeding, which usually occurs within 3-8 days after operation. If the latter is judged, it is recommended not to observe or be conservative, but to use absorbable suture to stop bleeding immediately under direct vision.
11. Why does RPH set the ligation point at 1.0cm of the dentate line instead of close to the dentate line?
As mentioned earlier, hemorrhoids (internal hemorrhoids) are actually lesions in the anal pad tissue (anal pad downward and varicose veins) (as shown in Figure 1). Ligation close to the dentate line will cause greater damage to the anal pad. When the ligation times are more, it is bound to damage the normal structure of the anal pad tissue, and thus damage the normal anal closure and defecation function. In addition, there are many specialized tissue structures near the dentate line, such as anal column, anal flap, anal papilla, anal gland, and various nerve receptors, which play an important role in defecation sensation, reflex, discrimination, closure and so on. Therefore, setting the ligation center at 1.0cm of the dentate line (equivalent to the upper part of hemorrhoids) is to avoid direct damage to the anal cushion tissue and the specialized structure near the dentate line, and to protect the normal anal closure and defecation function.
Secondly, close to the dentate line ligation, it is very easy to put the anal column or even dentate line into it, and the feeling of postoperative distension and urgency is obvious, sometimes even causing severe pain.
Finally, close to the dentate line ligation, such as the anal column or dentate line into which, because the place is not covered by the mucosa, but the transitional epithelium, the healing speed is slow, the infection rate is high, and the hemorrhoid tissue itself is extremely fragile, rich and varicose blood vessels, the incidence of postoperative bleeding is high.
12. What is the therapeutic principle of RPH?
The therapeutic principles of RPH are as follows
(1) Ligation of the base of hemorrhoid block made the internal hemorrhoid block ischemic, necrotic, collapse and fall off;
(2) Ligation of internal hemorrhoids can block (or partially block) hemorrhoid venous reflux at the same time, so as to reduce blood stasis;
(3) The ligation of hemorrhoid mucosa causes the mucosa to shrink, the anal pad to be lifted up, and the hemorrhoid mass to retract (according to our study, the ligated mucosa is about the size of the end of the little finger, and the expanded shape is disc-shaped, with a diameter of 2.5-3.0 cm);
(4) There is aseptic inflammatory reaction in the mucosa of the ligated hemorrhoids, which leads to the adhesion of the mucosa, submucosa and superficial muscle layer. The anal pad is fixed at a higher position to prevent the anal pad from sagging again and the recurrence of hemorrhoids.
In a word, the basic treatment principle of RPH can be summarized as two points: one is "lifting the anal pad" (that is, the mucosa shrinks after ligation, the anal pad is lifted up and fixed, and the hemorrhoids are retracted); The second is "collapse and disconnection" (that is, internal hemorrhoids collapse, blocking hemorrhoid venous reflux at the same time, reducing blood stasis). The treatment principle of PPH is only "lifting anal pad".
13. why does the rubber ring slide off immediately after the binding is completed?
After the binding is completed, the reasons for the immediate slippage of the rubber ring are as follows:
(1) Improper operation: because of the improper operation, the amount of tissue inhaled is too small, which makes the rubber ring not tight and slips off; Or repeatedly pull or rotate the anal peep during the binding, resulting in loose rubber ring due to friction.
(2) Too few suction tissue: too few tissues, the rubber ring is not tight, easy to slip off;
(3) Too low binding position: the lower the position, the greater the tension, the less easy the tissue to inhale, resulting in tight and loose rubber ring binding.
(4) The adjacent ligation point is too close: too close to the adjacent binding point will cause the mucosal tension to increase,
(5) Fibrosis or sclerosing of mucous membrane: for example, after PPH or injection treatment, the rectal wall must be fibrosis or sclerotic, which makes the tissue unable to inhale or inhale little, and the rubber ring is easy to slide off.
(6) Bad quality of rubber ring: the elastic force and shrinkage force of the rubber ring are poor, or the rubber ring aging will be caused by too long placement time, and it will easily slip off after binding.
Therefore, it is suggested to adopt the method of "ligation" and "injection", that is, after the completion of the ligation, inject 1-2ml of 1:1 mixture of "Xiaozhiling" or "Xiaozhiling + 2% lidocaine" in the tissue ball to make the rubber ring tighter and the possibility of slippage is very small.
14. when does the rubber ring fall off after RPH? How long is the risk period of bleeding? Can it cause anal edema?
After RPH, the time of the rubber ring falling off is 6-8 days, and a few days are 3-5 days (the stronger the retraction force of the rubber ring is, the earlier the time of falling off). This time is the peak of bleeding, so attention and prevention should be taken. However, there are also cases of bleeding 2 weeks later, which may be due to chronic ulcer and infection at the ligation point, or due to improper diet (such as drinking, eating spicy food, etc.) or dry and dry stool friction. However, as long as the RPH technology key points are properly grasped, and the rubber ring quality pass, bleeding can be completely avoided.
So, after the ligation can cause anal edema? unable! Because RPH fixed the insertion point at 1.5cm or higher on the dentate line, it had no effect on the venous and lymph flow of anal canal and anus, so it would not cause anal edema. At present, there is no clinical report of anal edema caused by ligation. However, it is important to remind that you should not tie the dentate line and anal skin, otherwise edema or even necrosis is completely possible, which must be paid great attention.
15. how much of the negative pressure value of RPH is more appropriate? Is it the greater the negative pressure is, the more tissue is inhaled?
The negative pressure suction value and the amount of tissue absorbed by RPH were gradually established after years of research. Theoretically, the larger the suction value of negative pressure, the more tissue is inhaled, but this is the case of ignoring the "barrel diameter". If the caliber of the barrel is taken into account, the same is true. According to the research, we set the diameter (inner diameter) of the barrel as 9.5mm, and the negative pressure suction value as -0.08 ~ -0.1mpa (this is the maximum negative pressure value of the commonly used electric negative pressure attractor in clinical practice). At this time, the tissue quantity of inhalation is basically fixed, that is, the size of the end segment (the straight diameter after deployment is 2.5-3.0cm). The clinical observation shows that the tissue size is suitable, which can achieve better therapeutic effect and not cause the patient to feel too strong discomfort (the more tissue inhaled, the more obvious the sense of falling swelling; If too much tissue is inhaled, it can even induce paroxysmal abdominal pain).
16. is RPH suitable for internal hemorrhoids, mixed hemorrhoids and circular hemorrhoids? How to treat external hemorrhoids after ligation?
RPH can be used for internal hemorrhoids, mixed hemorrhoids and ring prolapse hemorrhoids. Only the simple external hemorrhoids, embedded hemorrhoids and strangulated hemorrhoids without internal hemorrhoids are not suitable for RPH. If the mixed hemorrhoids are lighter, after RPH, because the anal pad is lifted, most of the external hemorrhoids can be automatically returned to the anus without additional treatment. Only when external hemorrhoids are varicose external hemorrhoids and are especially large, or inflammatory external hemorrhoids are formed, or thrombotic external hemorrhoids occur, they need to be treated separately (generally operated). RPH is feasible as usual for prolapse hemorrhoids, but one treatment may not be fully received, often need to be treated many times. The interval between two treatment was about one month. After 2-3 times of treatment, most of the prolapsed hemorrhoids can also be improved or cured.
For the fourth degree ring prolapse hemorrhoids, RPH should be performed after the anal expansion under local anesthesia, and it is often carried out in combination with external hemorrhoids resection. The specific method is to remove the varicose hemorrhoids with large volume and obvious prolapse. When removing, pay attention to protect skin as much as possible, and cut not too large and too wide, and do not cross the tooth line; The skin incision after hemorrhoids resection can be sutured by absorbable line (experience shows that "suture" is less painful and healing is faster than "non suture" wound). Then, three hemorrhoids were performed at 3, 7-8 and 11-12 (i.e. 1-2, 5-6 and 9 o'clock in knee and chest position) for three hemorrhoids (the binding position and the method of ligation can be determined according to the specific situation of the hemorrhoids). After the operation, prolapsed hemorrhoids can be basically returned to the anus.
In a word, RPH can do anything PPH can do.
17. can hemorrhoids be cured after RPH?
One of the first ideas to clarify here is that the principle of hemorrhoids treatment is not "radical treatment", but "eliminating symptoms". Must eliminate "see hemorrhoids cut" and "eliminate hemorrhoids" misunderstanding, "hemorrhoids can be cured?" Such problems themselves show that the principle of treatment for hemorrhoids is vague.
Hemorrhoids have two main symptoms: blood free and prolapse, which is the root cause of most patients. Any treatment method, as long as it can control "blood free" and "prolapse", it basically achieves the treatment purpose, not necessarily to eliminate "hemorrhoids". It should be known that the cost of eradicating hemorrhoids must be "damaging function". Remember, do not pursue the "beautiful appearance" of anus and cause serious damage to function. Only "eliminating symptoms" and "protection function" are the basic treatment of hemorrhoids.
18. how to evaluate hemorrhoids injection therapy? What are the advantages and disadvantages of RPH compared with it?
Hemorrhoids injection therapy is simple and easy to use, and it is also one of the traditional methods for hemorrhoids. But injection therapy has a obvious disadvantage, that is, pain or swelling after injection is obvious (lasting for 1-2 weeks or more), and almost all of them lead to sclerosing and scarring of rectum (PPH), which brings great trouble for the follow-up treatment. In addition, the rectal mucosa is easy to form ulcers after injection, and the incidence of infection is also high, which has a certain effect on defecation. There are even reports of rectal perforation, perianal infection and sepsis abroad. But the incidence of bleeding was low. At present, injection therapy has been eliminated in foreign countries.
Compared with injection therapy, RPH is not only easy to operate, good in effect, without any scar left after ligation, which brings great convenience to follow-up treatment, but also rarely complications. The only complication of RPH is accidental postoperative bleeding, which usually occurs in doctors without experience or experience. As long as the operation is proper and experienced, the bleeding complications of RPH can be avoided.
19. is RPH used for hemorrhoids treatment, and is there any other use?
RPH is mainly used for hemorrhoids treatment, but also for the treatment of rectal mucosa prolapse, local benign lesions (such as rectal polyps, rectal hemangioma or vascular malformation). In recent years, experts in some areas have used RPH in the treatment of "procedure rectocele", which is said to have achieved certain curative effect.
20. how should hemorrhoids patients cooperate with treatment? What should we pay attention to in the aspect of food and living?
Hemorrhoids is not a serious disease, but it often makes people restless. If it is not handled properly, it will bring some unexpected serious consequences. Therefore, in addition to believing in science and regular treatment, patients themselves should actively cooperate with doctors and carry out some necessary auxiliary treatment to achieve better results.
First, improper diet often leads to hemorrhoids attack or aggravation, so we must pay attention to diet. Try to avoid eating spicy food (such as spicy food), drink less (especially strong liquor), drink more water, and eat more food with high cellulose (such as vegetables and fruits).
Second, constipation is an important reason for the onset and attack of hemorrhoids, so it is very important to develop good defecation rules and habits, and pay attention to keep the stool unobstructed. If the stool is too dry, be sure to eat more food with high cellulose, drink more water, exercise properly, drink honey water often, or eat some bananas every day, which will help to soften the stool. However, if the problem can not be solved, it is necessary to take some drugs or laxatives to soften the stool properly under the guidance of doctors, but do not overdose and cause diarrhea, because diarrhea will also aggravate hemorrhoids. Of course, some constipation is pathological (such as rectocele, colon lengthy disease, etc.), we must ask the doctor to make a careful diagnosis, find out the reason, and carry out targeted treatment.
Third, the appropriate use of warm water sitting basin and anal movement is an effective auxiliary means of hemorrhoids treatment. The so-called sitting basin is to put the boiled warm water (as hot as possible, but not so hot) in the basin, add appropriate liquid medicine, and then sit in the basin with bare anus for 10-15 minutes, 2-3 times a day. Warm medicine can improve local blood circulation and promote the regression of inflammatory edema. The so-called anal relaxation movement is to use the muscles around the anus and perineum to consciously contract, relax, contract and relax... This is very good for improving the blood return of anus and rectum and reducing blood stasis. The above two auxiliary means can be combined, such as sitting basin while doing anal movement. It can also do anal movement when sitting or standing still.
Fourth, pay attention to anal and perineal hygiene, frequent bathing, avoid dirty sexual behavior (especially anal sex), strengthen physical exercise, avoid sedentary or long standing, local application of some effective anal suppository, etc., are conducive to the treatment and recovery of hemorrhoids.